Drug quantity limits: Why Zepbound jumped from $35 to $550
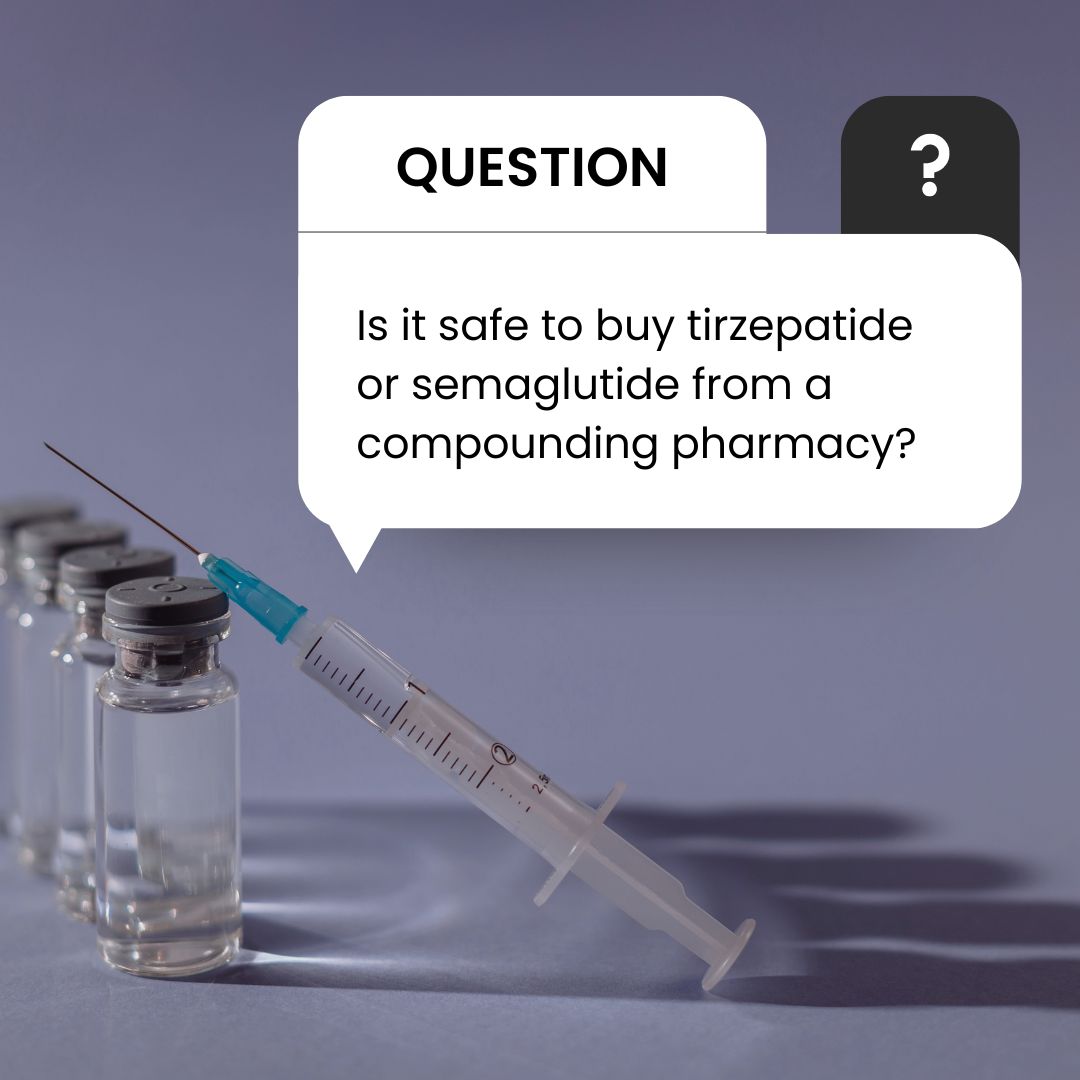
Readers often email me questions and I do my best to answer everyone who reaches out. Sometimes a question will resonate with a lot of people so when that happens, I post my response right here.
Last week, a reader wrote:
“Last month, I paid $35 for my first box of Zepbound 2.5mg. When I went to pick up my refill, the price skyrocketed to $550. The cashier couldn’t explain why. Do you know what’s going on here? I can’t afford to pay $550 for this medicine every month.”
Drug quantity limits: An insurance rule no one explains
I do have an idea of what’s going on in this situation. The same thing happened to me when my insurance company declined to cover my Zepbound 2.5mg refill. I called Express Scripts numerous times and no one could explain what was happening.
Related reading: Everything you need to know about Zepbound
I finally got a customer service agent who spent time on the phone with me while reading some internal documentation. She said insurance would only cover one box of 2.5mg. Even she didn’t think that made sense. But she told me that 5mg would be covered. Hmm. I asked if she could send me a copy of the document she was reading but she told me that wasn’t allowed. Double hmm.
After that phone call, I reviewed the denial letter that was in my Express Scripts online portal. I Googled this phrase from it:
“Coverage for additional drug quantities is provided when more than two consecutive doses are missed and re-initiation of treatment is needed.”
Express Scripts Notice of Adverse Benefit Determination
That’s when I hit paydirt. I found a document online that explained which doses were covered and to what extent in a calendar year by my insurer.
Here’s why this reader’s Zepbound 2.5mg refill wasn’t covered:
“Of note, the 2.5mg dose is for treatment initiation and is not intended for chronic weight management. The recommended maintenance doses of Zepbound are 5mg, 10mg, or 15mg SC QW.”
Cigna National Formulary Coverage – Policy: Weight Loss — Zepbound Drug Quantity Management
This chart appears later in this policy document and it outlines what my insurer will cover in terms of Zepbound doses:
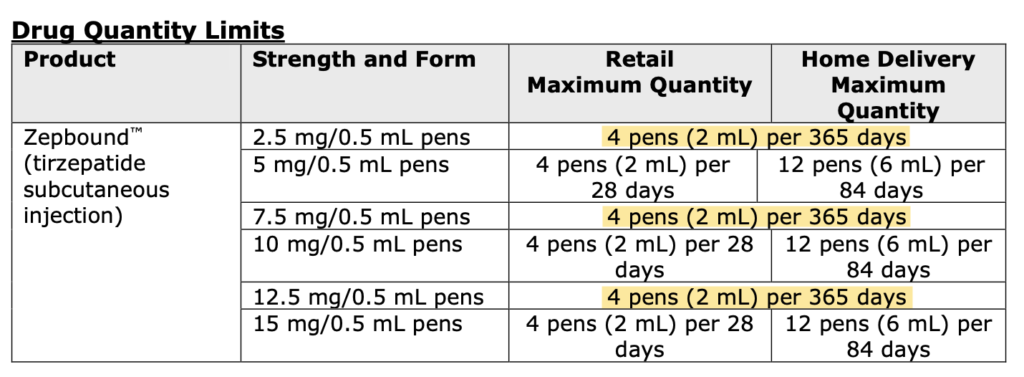
This shows that, for this insurance policy, the plan will only pay for one box of Zepbound 2.5mg, 7.5mg, and 12.5mg per 365 days. You can titrate up to the next dosage and it will be covered by insurance. This chart explains that you are covered for a refill of 5mg, 10mg, or 15mg every 28 days.
In this example, you can stay at the existing 2.5mg dose and pay out of pocket. In that scenario, your pharmacy can apply the manufacturer’s savings coupon to bring the cost down to $550 per box of Zepbound (four pens).
Request a PLA to override the drug quantity limit
You or your doctor can request something called a “PLA.” This is the paperwork asking your insurer to give you an exception to the drug quantity limit rule. My doctor and I both appealed the decision that led to my own refill coverage denial and both appeals were denied. In my case, I just paid the $550 to stay on 2.5mg for one more month. The following month I picked up a 5mg prescription and it was covered, as expected, by my insurer.
What if I can’t get my dose?
The way this policy is written, there’s the possibility of getting additional 2.5mg, 7.5mg, or 12.5mg refills covered if you first miss two consecutive doses. That might be something you need to investigate if you are on 10mg, for example, but the drug shortage keeps you from finding that dose for your refills.
If three weeks go by, your doctor will suggest going down a dose or restarting all the way back at 2.5mg (depending on your situation) instead of restarting 10mg. This is to avoid side effects. If this scenario occurs, call your insurance company to find out what the next steps are to get approved for a second pen at one of these lower doses (2.5mg or 7.5mg).
The wrap-up
Insurance coverage is complicated. Your best bet is to call your pharmacy benefits manager and ask a lot of questions about what is covered and if there are any limits. When my Zepbound prior authorization was approved, Express Scripts just said this medication was now covered. It did not explain any of the drug quantity limit rules. That would have been helpful.
What other insurance questions do you have? Send me a note or post it on the Shots to Shed Pounds Facebook page.